© 2025 NY4VEIN. All rights reserved.
DON'T JUST TAKE OUR WORD FOR IT
Stories That Inspire
The Few.
The Trusted.
The Vein Experts.
Inspiring Journeys, Real Results
Our Convenient Locations
Manhattan
30 Park Avenue
Mon-Fri: 9 AM-7 PM
Brooklyn
406 15th Street
Mon-Fri: 9 AM-7 PM
Brooklyn
44 Court Street, Suite 915
Mon-Fri: 9 AM-7 PM
Let our vein experts help you — Fill the Form to schedule your appointment!
* Vein treatment is not approved by the following carriers:
Fidelis, MetroPlus, HealthFirst and HealthPlus
How Poor Circulation Impacts Your Health
Poor circulation affects millions, yet many people don’t fully understand how it occurs or why it's important. Proper blood circulation is essential for maintaining overall health, and understanding its causes can help prevent and manage symptoms effectively.
The Role of Veins and Arteries in Circulation
Both veins and arteries are vital components in maintaining healthy blood flow, but their roles differ significantly:
- Arteries carry oxygen-rich blood from your heart throughout your body.
- Veins transport oxygen-poor blood back to your heart for re-oxygenation.
Your heart pumps blood through your arteries, but veins rely primarily on muscle movement and special valves, especially in your legs—to return blood upward against gravity.
Causes and Types of Poor Circulation
Poor circulation typically arises from issues within the arteries or veins, each leading to different complications:
Arterial Causes: Arterial Atherosclerosis & Peripheral Artery Disease (PAD)
Arterial atherosclerosis refers to fatty deposits (plaque) narrowing your arteries, decreasing the flow of oxygen-rich blood. This condition can lead to:
- Heart attacks, when arteries supplying the heart narrow.
- Strokes, if arteries supplying the brain narrow.
- Leg ulcers or gangrene, if leg arteries are affected.
Peripheral artery disease (PAD) is a common circulatory condition caused by atherosclerosis, characterized by:
- Pain or cramps while walking or resting.
- Slow-healing wounds.
- Serious complications, like infections or limb loss, if untreated.
Medical interventions such as stenting, angioplasty, or bypass surgery are often necessary to restore healthy blood flow.
Venous Causes: Venous Insufficiency
Venous insufficiency (also called venous incompetence or venous stasis vasculopathy) occurs when veins cannot effectively transport blood back to your heart, causing blood pooling in the legs. Common symptoms include:
- Leg pain or heaviness.
- Swelling, particularly after prolonged standing.
- Varicose veins.
- Skin changes, such as discoloration or ulcers.
Symptoms of Poor Circulation
Recognizing early signs helps you seek prompt care. Common symptoms include:
- Cold hands or feet.
- Numbness or tingling sensations.
- Pain or cramps, particularly in the legs.
- Swelling in lower extremities.
- Skin discoloration or varicose veins.
- Slow wound healing.
Preventing and Managing Poor Circulation
Simple lifestyle adjustments can improve circulation and reduce symptoms:
- Exercise regularly: Stimulates blood flow and strengthens your circulatory system.
- Eat healthily: A balanced diet reduces cholesterol, preventing arterial blockages.
- Avoid tobacco: Smoking constricts arteries, significantly worsening circulation problems.
- Wear compression stockings: Can reduce venous symptoms by improving circulation.
- Regular health check-ups: Early diagnosis and treatment help prevent severe complications.
Understanding Vein Disease and Circulation Health
How Veins and Arteries Affect Your Health
Veins and arteries work continuously to transport blood throughout your body:
- Arteries carry oxygen-rich blood from your heart to all body tissues.
- Veins return oxygen-poor blood back to your heart.
While arteries benefit from the heart’s pumping action, veins depend significantly on muscle contractions and specialized venous valves—especially in your legs. Due to our upright posture, veins in the legs face extra pressure, highlighting the importance of healthy venous valve function.
Common Conditions Linked to Vein Disease and Circulation Problems
Circulation problems often impact your overall health, contributing to various vascular conditions. Common circulation-related issues include:
- Venous Insufficiency and Chronic Venous Insufficiency (CVI)
Occurs when vein valves malfunction, causing blood to pool and veins to enlarge or weaken, potentially leading to varicose veins or skin ulcers. - Arterial Atherosclerosis
Fatty deposits (atherosclerosis) narrow arteries, restricting blood flow and potentially causing:- Heart attacks (when coronary arteries are affected)
- Strokes (when cerebral arteries are affected)
- Trophic ulcers and gangrene (when leg arteries are involved)
- Peripheral Artery Disease (PAD)
A condition characterized by reduced arterial blood flow to legs, often causing pain, wounds that heal slowly, and difficulty walking or exercising.
Why Healthy Circulation is Crucial for Healing and Overall Wellness
Impaired circulation can significantly impact healing processes:
- Reduced blood supply slows down tissue repair, affecting recovery after surgeries and injuries.
- PAD patients typically experience slower wound healing due to insufficient blood flow, which can complicate overall treatment.
The body may attempt to adapt by developing collateral (new) blood vessels. Unfortunately, these compensations rarely restore optimal blood flow, especially during physical activities or stress. Medical treatments such as angioplasty, stenting, or bypass surgery often become necessary.
Managing and Preventing Vein Disease and Circulation Problems
Taking proactive steps can help manage and even prevent many circulation-related conditions:
- Stay Active
Regular, moderate exercise promotes better blood flow and strengthens vein walls. - Healthy Diet
Eating nutritious foods low in unhealthy fats can minimize arterial plaque buildup. - Quit Smoking
Smoking damages blood vessels and significantly increases risk for circulation problems. - Routine Check-Ups
Regular screenings by a vascular specialist can detect early signs, allowing for timely intervention and improved outcomes.
Vein Treatments in NYC: Advanced, Minimally Invasive Solutions
At New York Vein Treatment Center, we specialize in minimally invasive vein treatments that relieve symptoms, improve circulation, and restore your quality of life. We provide customized care in Manhattan, Brooklyn, Queens, Staten Island, and surrounding areas.
Varicose Vein Treatment
Varicose veins are symptoms of venous insufficiency, a condition where veins fail to circulate blood properly. Untreated, this can cause ulcers, blood clots, and infections. Our minimally invasive varicose vein treatments quickly relieve discomfort and restore healthy circulation.
Endovenous Laser Therapy (EVLT)
EVLT is an advanced, minimally invasive varicose vein treatment. A small catheter delivers laser energy to seal the diseased vein from the inside, redirecting blood flow into healthy veins.
Benefits of EVLT include:
- Immediate symptom relief
- Quick recovery with minimal discomfort
- No hospitalization required
ClariVein Treatment (Mechano-Chemical Ablation)
ClariVein treatment combines mechanical and chemical vein closure without heat, ideal for sensitive patients or veins located in difficult areas.
Key features:
- No thermal trauma (heat)
- Performed under local anesthesia
- Reduced risk in select patients
However, careful evaluation is essential due to possible vein reopening (recanalization).
Varithena Treatment (Foam Sclerotherapy)
Varithena is an FDA-approved foam sclerosant used to close diseased veins effectively. Guided by ultrasound, Varithena safely collapses veins and redirects blood flow.
Advantages include:
- Quick and virtually painless
- No incisions or general anesthesia
- Suitable for twisted, complicated veins
VenaSeal Treatment (Medical Adhesive)
The VenaSeal procedure uses a safe medical adhesive to permanently close varicose veins. A small catheter precisely delivers adhesive, redirecting circulation to healthy veins.
Key benefits:
- Minimal discomfort, no downtime
- Immediate improvement in symptoms
- No need for compression stockings afterward
Radiofrequency Ablation (RFA)
RFA treatment seals veins using heat generated by radiofrequency energy. It's highly effective for treating chronic venous insufficiency.
Benefits:
- Minimally invasive with rapid recovery
- High success rate
- Local anesthesia only
Microphlebectomy (Ambulatory Phlebectomy)
Microphlebectomy removes visible varicose veins through tiny incisions. Typically combined with other treatments, it's ideal for larger, prominent veins.
Advantages include:
- Minimally invasive outpatient procedure
- Quick symptom relief
- Minimal scarring
Spider Veins Treatment Clinic in NYC
Spider veins (thin red, blue, or purple veins) typically appear around knees, calves, and ankles. Often a symptom of underlying vein disease, they require professional evaluation to prevent recurrence.
Our spider veins treatment clinic offers comprehensive care to permanently eliminate spider veins and address underlying conditions.
Sclerotherapy Treatment Clinic: Effective Spider Vein Removal
Sclerotherapy injects a specialized solution (sclerosant) into spider veins, causing them to close and fade away. It's ideal for reticular and spider veins.
Benefits include:
- Quick outpatient procedure
- High success rate
- Minimal discomfort and downtime
Dornier FlexiPulse: Non-Invasive Spider Vein Laser Treatment
Dornier FlexiPulse is a completely non-invasive laser treatment that eliminates small spider veins safely, quickly, and painlessly. It's perfect for smaller, superficial veins.
Key features:
- No needles or incisions
- Immediate visible results
- Painless and safe
Compression Therapy for Venous Disorders
Compression therapy uses special stockings or bandages that gently squeeze your legs, improving circulation and relieving symptoms like swelling, heaviness, and discomfort.
Important notes:
- Provides temporary symptom relief
- Not a permanent cure alone, typically combined with other treatments
- Custom-fitted stockings are most effective
Lifestyle Modification to Improve Vein Health
Lifestyle changes can significantly enhance treatment outcomes and prevent recurrence:
- Regular exercise focusing on leg and calf muscles
- Maintaining a healthy weight
- Elevating legs to reduce pressure and swelling
- Avoiding prolonged standing or sitting
Varicose Veins Treatment Clinic
What Causes Varicose Veins?
Varicose veins, also called varicosities, aren't merely a cosmetic concern—they signal an underlying condition called chronic venous insufficiency (CVI). This condition occurs when the one-way valves in your veins fail, causing blood to pool instead of flowing smoothly back to your heart.
Key causes and risk factors include:
- Genetics (family history)
- Aging
- Pregnancy
- Obesity
- Prolonged standing or sitting
Recognizing these factors helps in both prevention and effective treatment.
Signs You Might Have Varicose Veins or CVI
It's essential to differentiate between normal veins and varicosities:
- Normal veins: Usually straight, smooth, and even slightly bulging without symptoms.
- Varicose veins: Typically twisted, enlarged, and associated with symptoms such as:
- Leg heaviness or aching
- Swelling and cramping
- Itching or skin discoloration
- Restless legs, pins-and-needles sensation, or numbness
Effective Treatment for Varicose Veins and CVI
Our varicose veins treatment clinic specializes in diagnosing and treating the root cause of varicose veins—chronic venous insufficiency. Treating CVI directly addresses symptoms and prevents serious complications like:
- Blood clots (deep vein thrombosis, or DVT)
- Venous ulcers (open wounds)
- Bleeding and infections
- Skin conditions and discoloration
We use advanced diagnostic methods and personalized treatments to effectively address your condition and restore your leg health.
Why Choose Our Varicose Veins Treatment Clinic?
Patients from Manhattan, Brooklyn, and throughout NYC trust our clinic because we offer:
- Comprehensive diagnosis: Using ultrasound imaging to accurately detect valve dysfunction.
- Minimally invasive treatments: Procedures like Endovenous Laser Therapy (EVLT), sclerotherapy, and vein ablation.
- Expert vascular specialists: Dedicated team experienced in treating chronic venous insufficiency and varicose veins.
Understanding Chronic Venous Insufficiency (CVI)
CVI affects millions yet remains poorly understood. This condition, also known as superficial venous insufficiency or chronic venous hypertension, results from malfunctioning venous valves. Blood flows backward, increasing vein pressure, causing symptoms such as:
- Varicose and spider veins
- Persistent leg pain or heaviness
- Swelling and muscle fatigue
- Skin ulcers and infections (if untreated)
Early treatment at a specialized varicose veins treatment clinic helps prevent serious complications.
How to Prevent Varicose Veins and CVI
While not entirely preventable, lifestyle adjustments can significantly lower your risk:
- Regular exercise, especially walking or swimming
- Avoid prolonged sitting or standing
- Maintain a healthy weight
- Wear compression stockings, if recommended by a doctor
Spider Veins Treatment Clinic in NYC: Effective, Minimally Invasive Solutions
Understanding Spider Veins
Spider veins are small, thin veins that appear red, blue, or purple beneath your skin, often found around the knees, calves, and ankles. They can result from dilated capillaries close to the skin’s surface.
Common reasons for developing spider veins include:
- Genetics and family history
- Aging
- Hormonal fluctuations (pregnancy, menopause)
- Prolonged standing or sitting
- Obesity
It's crucial to know that spider veins can indicate deeper venous issues. At our Spider Veins Treatment Clinic, we don't just address cosmetic concerns—we investigate and treat underlying vein conditions to ensure long-lasting results.
What is Sclerotherapy for Spider Veins?
Sclerotherapy is an effective, minimally invasive treatment for spider veins. It involves injecting a special solution, called a sclerosant, into affected veins, causing them to collapse and gradually fade away.
Benefits of sclerotherapy:
- Quick outpatient procedure
- Minimal discomfort
- Noticeable cosmetic improvement
- Effective for larger spider veins and reticular veins
Before undergoing sclerotherapy, identifying and treating underlying venous insufficiency is important to ensure lasting results.
Dornier Flexipulse Laser: Non-Invasive Spider Vein Treatment
For smaller spider veins, we utilize the advanced Dornier Flexipulse laser system, the only truly non-invasive treatment available today. Unlike traditional lasers, Dornier Flexipulse treats veins externally—no needles required.
Advantages of the Dornier Flexipulse treatment:
- No needles or incisions required
- Virtually painless procedure
- Fast sessions, typically under 30 minutes
- Effective treatment for tiny spider veins (telangiectasia)
It's important to remember that addressing the underlying cause of spider veins is crucial for optimal, long-term outcomes.
Why Choose Our Spider Veins Treatment Clinic?
When it comes to treating spider veins effectively, expertise and experience matter. At our New York vein center, you're in trusted hands with:
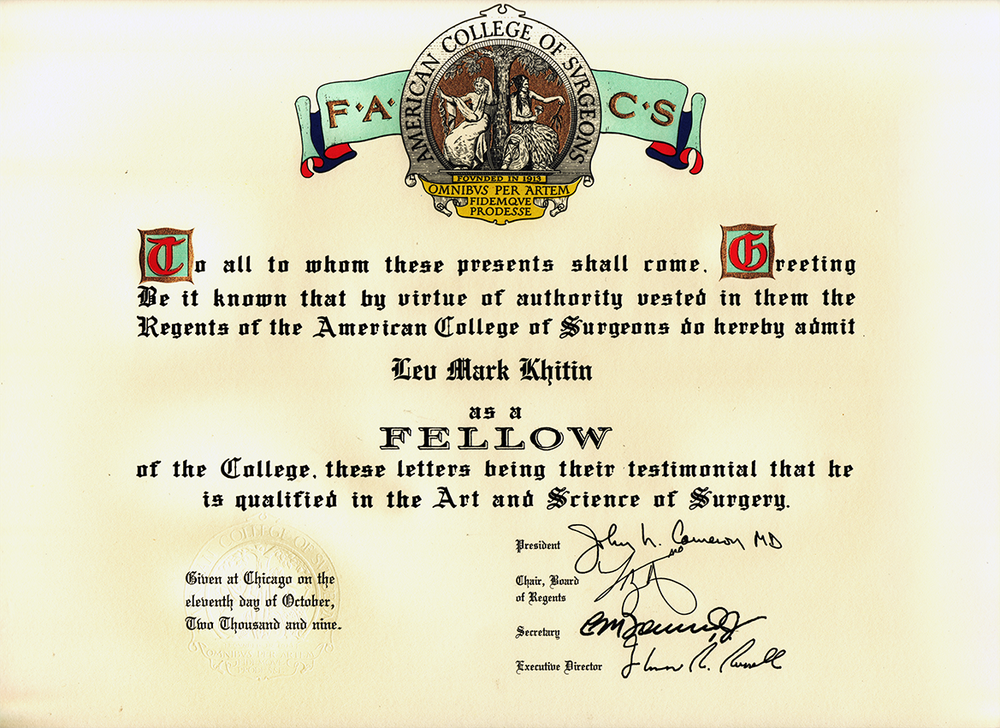
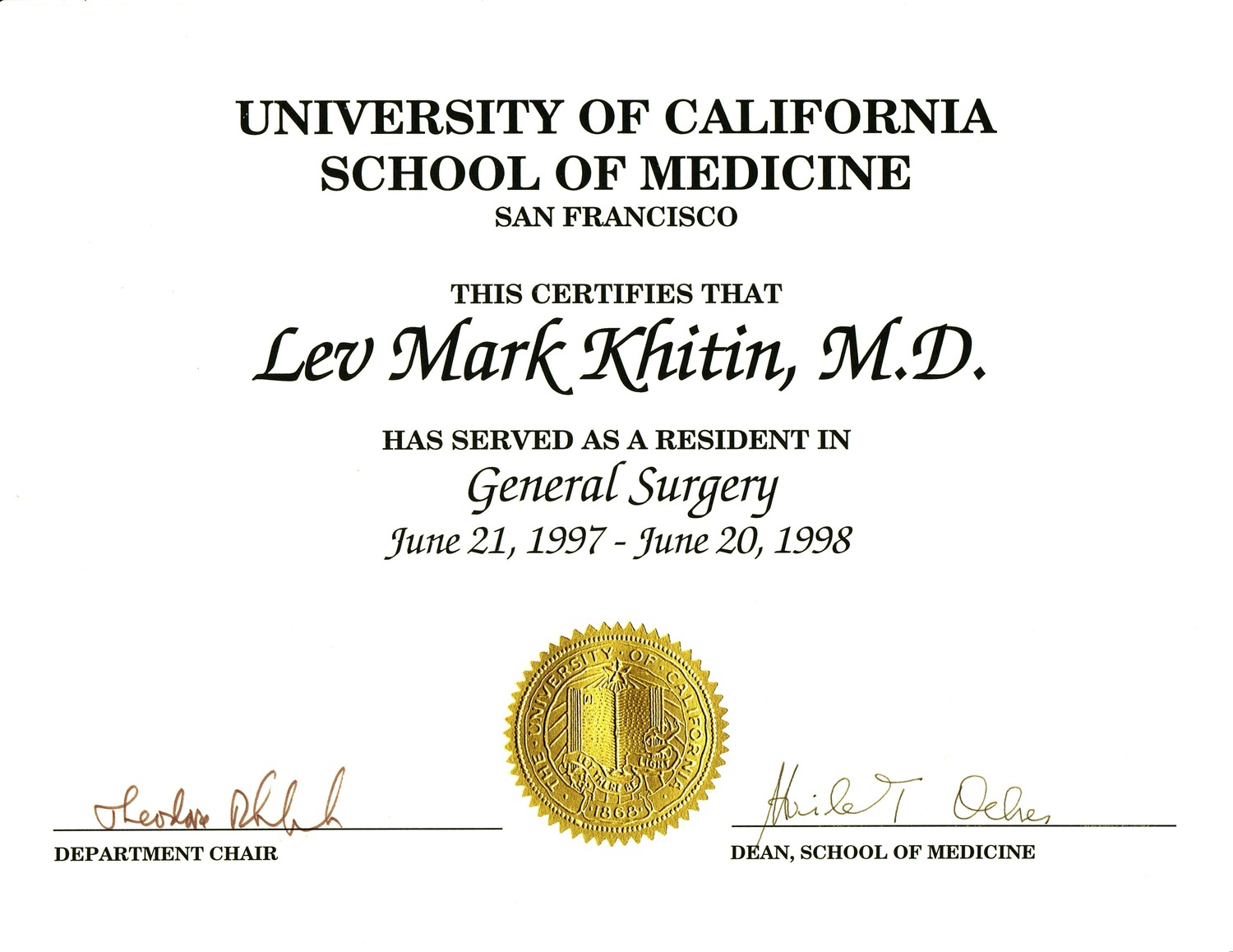
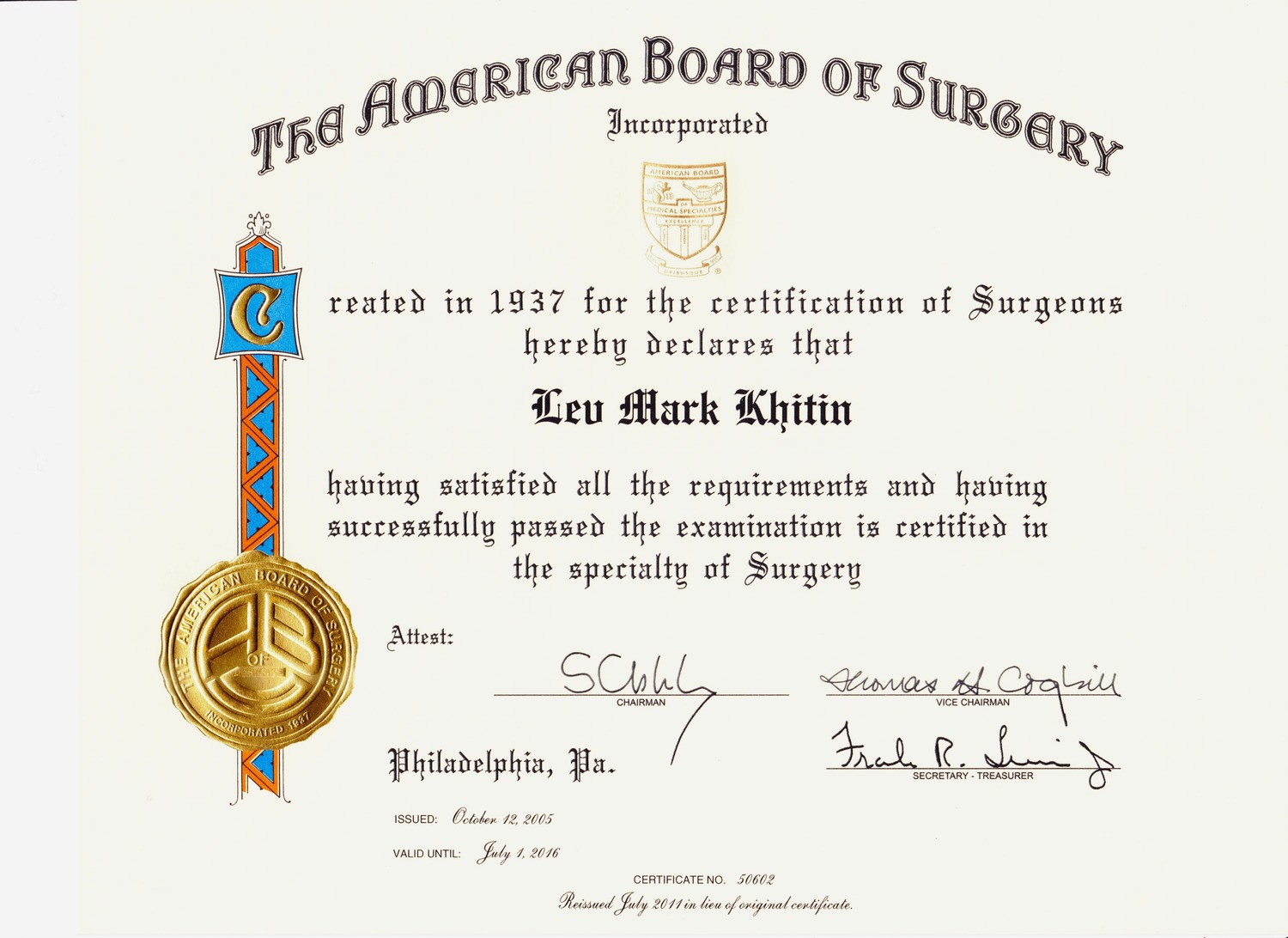
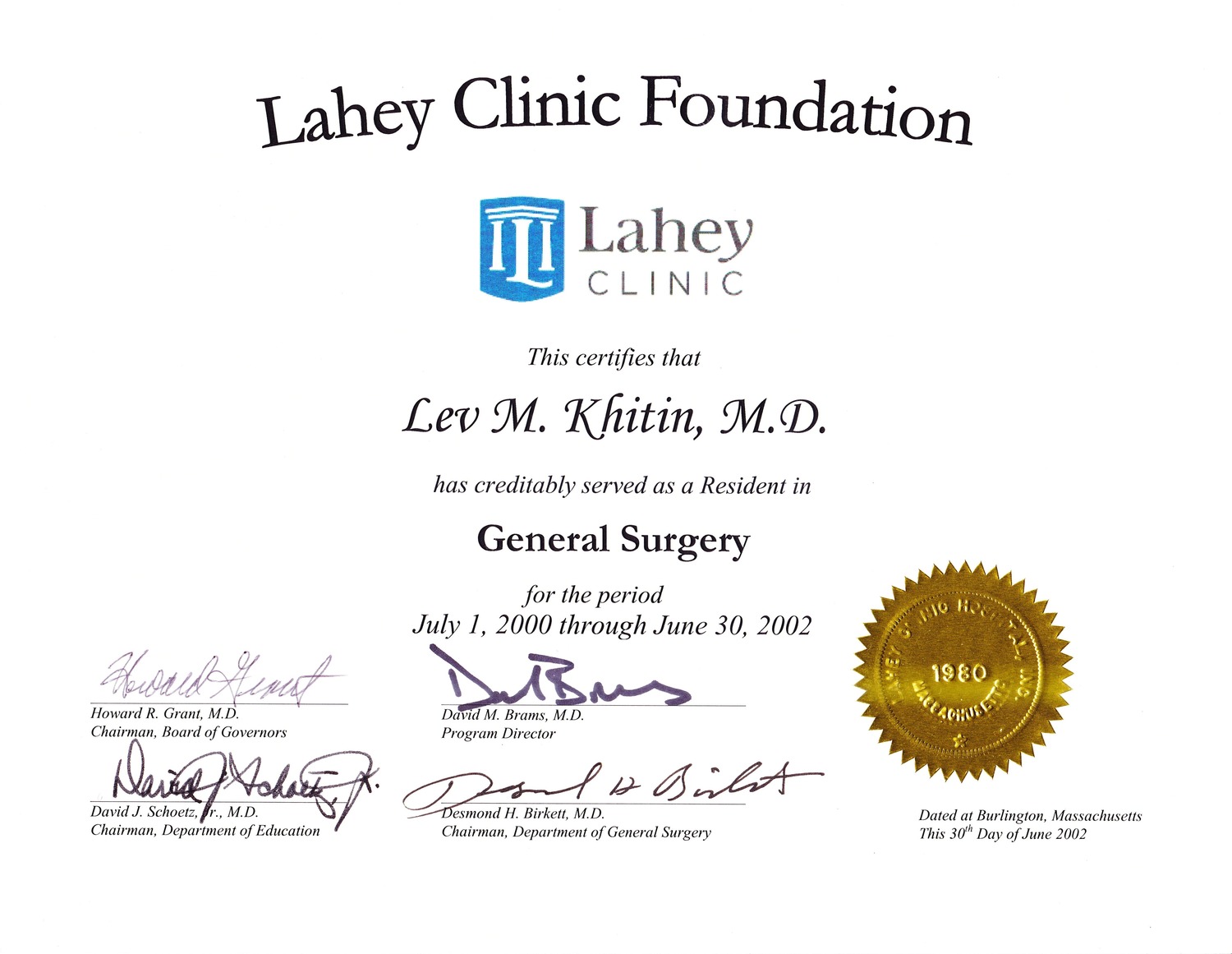
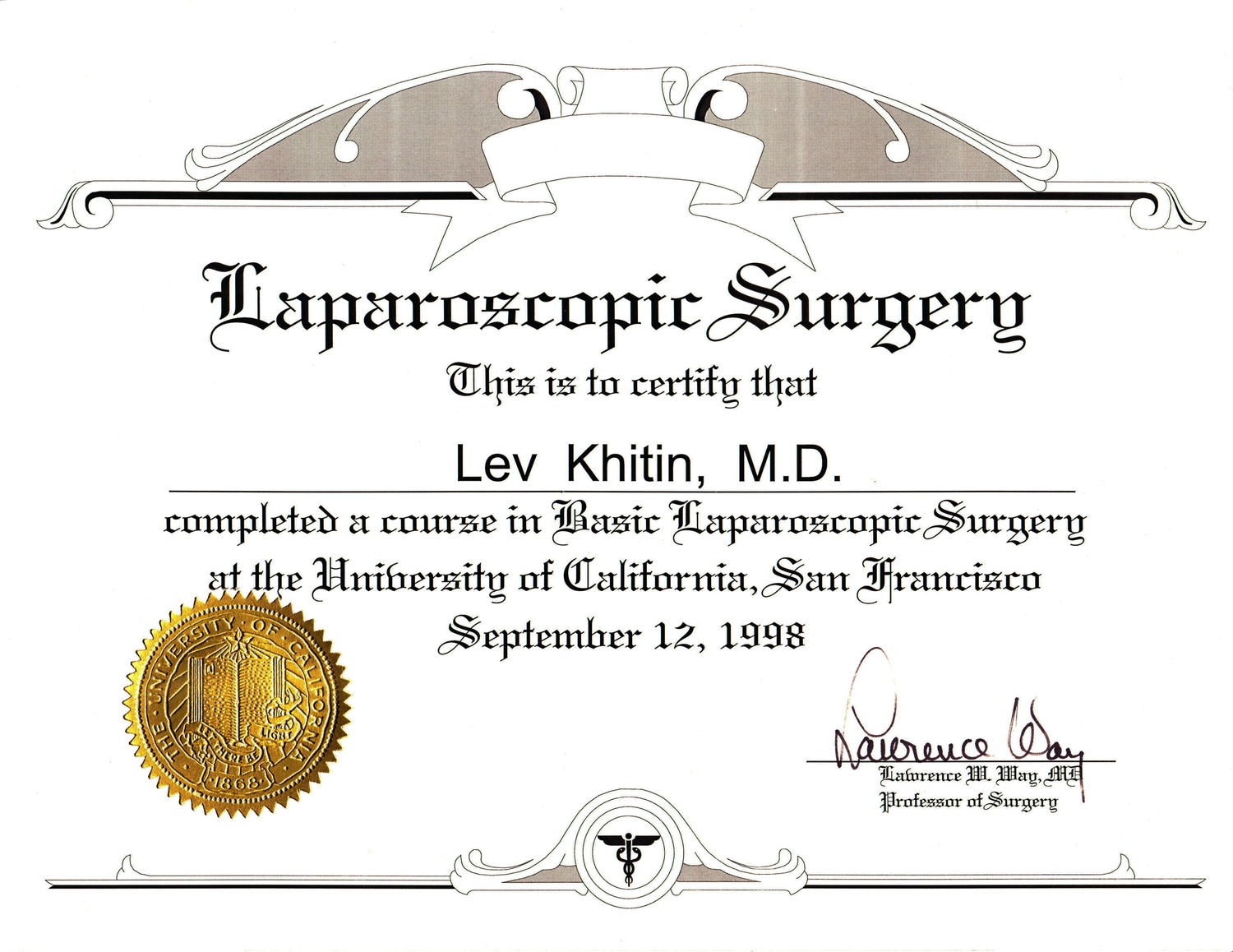
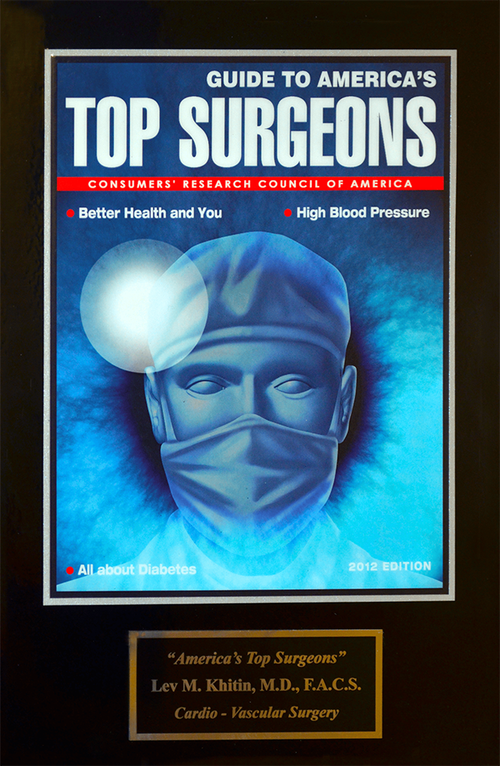
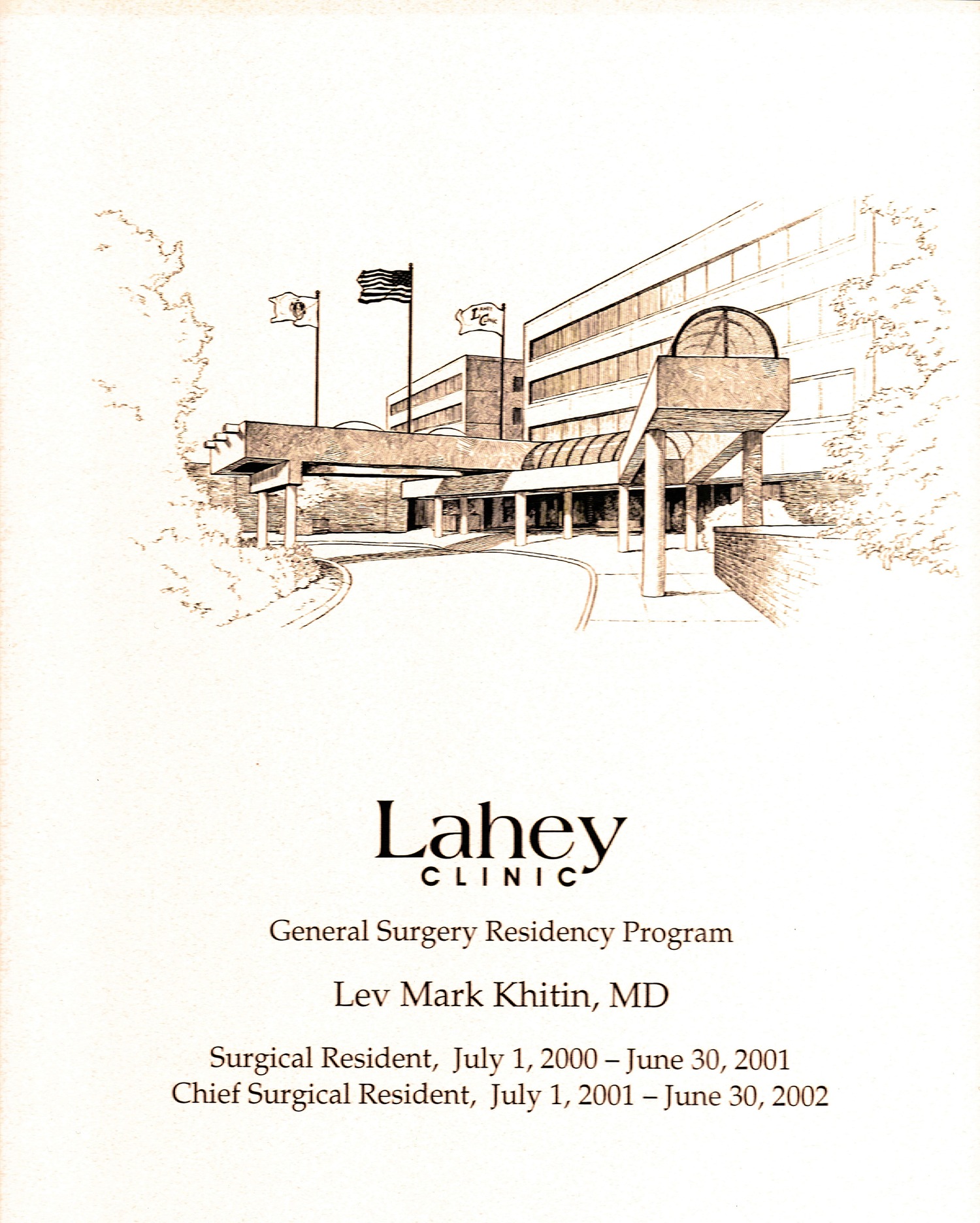
- Renowned Specialist:
Dr. Khitin, a highly respected expert in vascular medicine, venous disorders, phlebology, and cardiovascular health. - Comprehensive Diagnosis & Treatment:
We offer thorough vein evaluations to accurately diagnose underlying issues and provide individualized treatments tailored specifically to your needs. - Advanced Minimally Invasive Procedures:
Our clinic uses cutting-edge technology and methods, ensuring your treatment is safe, effective, and comfortable. - Convenient Locations:
With locations in Manhattan, Brooklyn, and across NYC, our specialized care is easily accessible.
Chronic Venous Insufficiency Specialist in NYC
If you're experiencing discomfort in your legs, consulting a Chronic Venous Insufficiency Specialist is essential for accurate diagnosis, effective treatment, and symptom relief. At our vein clinic in Manhattan, Brooklyn, and NYC, our specialists offer expert care tailored to your needs.
What is Chronic Venous Insufficiency (CVI)?
Chronic venous insufficiency (CVI), also known as superficial venous insufficiency or chronic venous hypertension, occurs when your leg veins struggle to return blood to the heart efficiently.
This condition arises from faulty valves within the veins, allowing blood to flow backward and pool in your legs. CVI can often exist quietly, causing few noticeable symptoms early on. Common symptoms include:
- Aching, heavy legs
- Swelling and fatigue
- Varicose veins or spider veins (though sometimes invisible)
- Itching or skin discoloration
- Leg cramps or restless legs
Many people have CVI without visible signs, which is why seeing a chronic venous insufficiency specialist is crucial for early diagnosis and treatment.
Why Should You Consult a Chronic Venous Insufficiency Specialist?
A chronic venous insufficiency specialist offers advanced diagnostic skills and targeted treatments to address CVI at its source, rather than just managing symptoms. Seeking specialized care is particularly important if you experience:
- Persistent leg swelling and heaviness
- Unexplained pain or aching in legs
- Skin discoloration or texture changes
- Development of varicose or spider veins
- Slow-healing wounds or leg ulcers
Early intervention by a CVI specialist significantly reduces the risk of severe complications such as ulcers, blood clots, bleeding, infections, or skin conditions.
Potential Complications if CVI is Left Untreated
Without proper treatment, chronic venous insufficiency can progress to serious complications:
- Venous leg ulcers: Open wounds resulting from persistent elevated pressure in leg veins, difficult to heal without specialized care.
- Blood clots (Deep Vein Thrombosis): Increased risk due to stagnation of blood flow.
- Bleeding and skin infections: Resulting from skin changes and weakened tissues.
- Chronic swelling and discomfort, reducing overall quality of life.
Effective Treatments Offered by a Chronic Venous Insufficiency Specialist
Our clinic provides state-of-the-art treatments designed specifically for CVI:
- Endovenous Laser Therapy (EVLT): Minimally invasive laser procedure to close diseased veins.
- Radiofrequency Ablation (RFA): Uses heat to seal affected veins.
- Sclerotherapy: Injection therapy for eliminating diseased veins.
- Lifestyle Management and Compression Therapy: Supporting long-term venous health.
Our specialists personalize treatment plans based on your individual needs to ensure lasting relief.
How to Prevent Chronic Venous Insufficiency and Improve Vein Health
You can lower your risk and manage symptoms by:
- Regular physical activity like walking or cycling
- Maintaining a healthy weight
- Elevating your legs periodically
- Wearing compression stockings as recommended
- Avoiding prolonged sitting or standing
Recognizing Symptoms of DVT in the Legs: What You Need to Know
Deep Vein Thrombosis (DVT) occurs when a blood clot forms in a deep vein—commonly in the legs. Knowing the symptoms of DVT in the legs can help you seek prompt medical care, potentially preventing severe complications.
Common Symptoms of DVT in the Legs
While some cases may have no obvious symptoms, typical signs of DVT include:
- Leg swelling, usually affecting one leg
- Pain or tenderness in your leg, often described as cramping or soreness
- Warmth and redness around the affected area
- Heaviness or fatigue in the leg
- Skin discoloration or noticeable changes in skin texture
If you experience any of these symptoms, consider seeking immediate medical attention from a specialist.
DVT Complications: Why Early Diagnosis is Essential
DVT can lead to serious complications if left untreated, including:
- Pulmonary Embolism (PE): A life-threatening condition occurring when a clot breaks loose and travels to the lungs. DVT and PE together are called venous thromboembolism (VTE), affecting around 900,000 Americans annually.
- Post-Thrombotic Syndrome (PTS): A long-term condition resulting from damaged vein valves, causing chronic leg pain, swelling, skin changes, and ulcers. Approximately 60% of DVT patients experience PTS.
Risk Factors for DVT
Several factors increase the risk of developing DVT:
- Family history or blood clotting disorders
- Prolonged immobility (long flights, bed rest)
- Recent surgery or injury
- Smoking
- Pregnancy and postpartum period
- Advanced age (60+)
- Obesity
- Cancer diagnosis
- Hormone medications (birth control, hormone replacement therapy)
Awareness of these risk factors can help with early detection and prevention.
What is the Treatment for DVT in Legs?
Effective treatments for DVT aim to prevent complications and relieve symptoms. Common treatments include:
- Blood-thinning medications (anticoagulants)
Help prevent clot enlargement and new clot formation. - Thrombolysis and Thrombectomy (clot removal)
Minimally invasive procedures using catheters and medication to dissolve or remove blood clots. - Inferior Vena Cava (IVC) Filter
A filter device placed inside a major vein to prevent blood clots from reaching the lungs in patients who cannot take blood thinners.
Consulting a specialist ensures personalized, effective treatment based on your specific needs.
When Should I See a Doctor for Symptoms of DVT?
You should contact a specialist immediately if:
- You experience persistent swelling or pain in your legs.
- Your symptoms interfere with daily activities.
- Pain and swelling continue even after rest or leg elevation.
Early consultation and diagnosis by a vein specialist can prevent severe complications such as nerve damage, skin ulcers, or permanent leg damage.
Why Choose New York Vein Treatment Center?
At the New York Vein Treatment Center, we specialize in diagnosing and treating the symptoms of DVT in the legs. Our highly experienced vein specialists offer:
- Personalized care plans
- State-of-the-art treatments
- Comprehensive support to improve your quality of life
Understanding Reticular Veins, Venous Hypertension, and Chronic Venostasis
Reticular Veins: What Are They?
Reticular veins serve as connectors within your vascular system, moving blood from smaller surface veins to larger, deeper ones. Normally hidden, these veins sometimes appear visibly bluish-green under the skin, particularly in the legs or forearms.
When affected by venous insufficiency, reticular veins can expand and form varicose veins, leading to cosmetic issues and discomfort. Treating reticular veins effectively involves addressing any abnormal veins contributing to this issue.
Common symptoms of reticular veins:
- Bluish-green veins under the skin
- Cosmetic concerns
- Occasional mild discomfort or heaviness
Venous Hypertension: Causes, Types, and Complications
Venous hypertension refers to increased pressure within the veins, especially in the legs. It is separate from arterial hypertension (high blood pressure), which involves arteries.
There are two main types of venous hypertension:
- Primary venous hypertension: Caused by vein-related problems like deep vein thrombosis (DVT) or hereditary venous insufficiency.
- Secondary venous hypertension: Occurs due to external factors or underlying medical conditions, such as heart or kidney failure, fluid overload after transfusions, chemotherapy, or shock.
Risk factors and causes for venous hypertension include:
- Prolonged standing or heavy lifting
- Hereditary predisposition
- History of blood clots or vein injuries
- Fluid retention disorders (heart or kidney conditions)
Venous hypertension is serious if left untreated. Early diagnosis and proactive treatment are vital to prevent complications like ulcers, blood clots, infections, and long-term vein damage.
Chronic Venostasis: Understanding Venous Flow Abnormalities
Chronic venostasis, also called chronic venous stasis, describes impaired blood flow in veins, usually in the lower extremities. While related, it's distinct from chronic venous insufficiency.
Differences include:
- Chronic venous insufficiency: Veins dilate, causing backward (retrograde) blood flow away from the heart.
- Chronic venostasis: Blood moves sluggishly yet in the correct (antegrade) direction towards the heart, though under abnormally high pressure.
Chronic venostasis typically affects deep veins, which cannot dilate easily due to surrounding muscle tissues. It often arises from conditions other than blood clots (DVT), distinguishing it from post-thrombotic syndrome.
Symptoms can include:
- Persistent leg heaviness or aching
- Chronic swelling
- Skin discoloration or changes
- Risk of skin ulcers due to poor circulation
Identifying the underlying cause is crucial for effective treatment and long-term management.
Lymphedema Treatment Clinic
If you're experiencing swelling, heaviness, or discomfort related to lymphedema, our specialized lymphedema treatment clinic in Manhattan, Brooklyn, and NYC can help. Early diagnosis and effective treatment significantly improve your quality of life.
What are the Symptoms of Lymphedema?
Lymphedema is characterized by the buildup of lymph fluid in tissues, causing swelling. Recognizing symptoms early helps you get timely care:
- Swelling of arms or legs, including fingers or toes
- Feelings of heaviness or tightness
- Limited range of motion
- Frequent skin infections
- Thickened or hardened skin (fibrosis)
If you notice persistent limb swelling or sudden increases in size, contact our lymphedema treatment clinic immediately.
What Causes Lymphedema?
Lymphedema develops when lymph vessels or nodes cannot properly drain fluid, often due to:
- Cancer: Tumors blocking lymph vessels
- Cancer Treatments: Radiation or surgery involving lymph nodes
- Parasites: Filarial worms transmitted by mosquitoes in tropical regions
- Congenital Conditions: Inherited lymphatic system defects
In developed regions like NYC, lymphedema often results from surgery or cancer treatments. Early intervention at our clinic helps prevent complications and progression.
Why Choose Our Lymphedema Treatment Clinic?
New York Vein Treatment Center offers expert diagnosis and care for lymphedema and related conditions. Led by Dr. Khitin, an established expert in venous disorders, cardiovascular, and thoracic medicine, we’ve successfully treated thousands of patients throughout NYC.
Benefits of choosing us:
- Expert diagnosis and personalized treatment plans
- Convenient locations in Manhattan, Brooklyn, and NYC areas
- Comprehensive management of symptoms and related complications
May Thurner Syndrome: Symptoms, Causes, and Treatment
What is May-Thurner Syndrome?
May-Thurner Syndrome (MTS), also known as Iliac Vein Compression Syndrome or Cockett’s Syndrome, is a condition where the left iliac vein in the pelvis is compressed by the right iliac artery. This compression restricts blood flow from the left leg back to the heart, increasing the risk of complications like deep vein thrombosis (DVT) and venous insufficiency.
Symptoms of May-Thurner Syndrome
Symptoms of May-Thurner Syndrome often vary, and some individuals may experience none. However, common symptoms include:
- Leg swelling, often noticeable in just one leg
- Chronic leg pain or heaviness
- Skin discoloration (hyperpigmentation)
- Weakness in the legs when sitting or standing
- Varicose veins development
- Slow-healing venous ulcers due to elevated venous pressure
Women between 20 and 40 years old are most frequently affected, often due to pelvic pressure during pregnancy.
May-Thurner Syndrome and DVT
May-Thurner Syndrome significantly increases your risk of deep vein thrombosis (DVT)—a serious condition involving blood clots in the deep veins. Around 2-5% of all DVT cases are related to MTS. Untreated DVT can result in a potentially life-threatening complication called pulmonary embolism (PE), where a clot travels to the lungs, requiring immediate medical care.
Diagnosis and Treatment of May-Thurner Syndrome
Early diagnosis and treatment of May-Thurner Syndrome can prevent serious complications. Your doctor will typically use:
- Diagnostic venous ultrasound
- Venogram (specialized vein X-ray)
- Intravenous ultrasound (IVUS)
Once confirmed, effective treatments for MTS include:
- Anticoagulant (blood-thinning) medications
- Compression stockings
- Minimally invasive endovenous treatments, such as stenting, to relieve vein compression
Superficial Thrombophlebitis: Understanding Symptoms, Causes, and Risks
Superficial thrombophlebitis (ST), commonly known simply as thrombophlebitis, is an inflammation and clot formation occurring in veins just below the skin's surface. It frequently arises as a complication of chronic venous insufficiency, a condition where veins fail to properly circulate blood.
Although unpleasant and uncomfortable, superficial thrombophlebitis is typically not dangerous. However, many people confuse it with deep vein thrombosis (DVT), which can pose serious health risks.
Symptoms of Superficial Thrombophlebitis
Typical symptoms of superficial thrombophlebitis include:
- Swelling near the affected vein
- Visible redness and tenderness to touch
- Warmth and discomfort along the vein
- Pain or aching in the affected area
These symptoms arise from the inflammation caused by thrombophlebitis, distinguishing it clearly from DVT.
Superficial Thrombophlebitis (ST) vs. Deep Venous Thrombosis (DVT)
It's crucial to understand the differences between superficial thrombophlebitis and deep vein thrombosis:
- Superficial Thrombophlebitis (ST):
- Occurs in veins close to the skin’s surface.
- Includes inflammation, redness, tenderness, and warmth.
- Generally not life-threatening and rarely causes serious complications.
- Deep Venous Thrombosis (DVT):
- Affects veins located deeper in the body, usually in legs.
- Does not typically cause redness or visible inflammation.
- Can lead to pulmonary embolism (PE), a serious, potentially life-threatening condition if a clot moves to the lungs.
It's important to consult a vein specialist if you're experiencing any symptoms to rule out potentially serious issues like DVT.
Hand Veins: Causes and Effective Treatment Options
Prominent hand veins are common as we age, resulting from decreased collagen production and loss of fat under the skin. This makes veins more visible and skin appear thin and less elastic. Although bulging hand veins typically aren't diseased or varicose, many find them cosmetically unappealing.
At New York Vein Treatment Center, our experts offer effective treatments for hand veins, including:
- Sclerotherapy: A minimally invasive injection therapy to remove visible veins.
- Mini micro-phlebectomy: Surgical removal of veins through tiny incisions, used occasionally.
Schedule a consultation to discover the best solution for your hand veins.
Face Veins: Effective Treatments for Spider Veins on the Face
Visible face veins, also called facial spider veins or telangiectasia, appear as thin, red, or purple lines around the nose and cheeks. Common causes include:
- Aging and loss of skin elasticity
- Hormonal changes
- Excessive sun exposure
- Fair skin complexion
Although facial veins usually aren't medically harmful, they can impact your self-esteem.
At New York Vein Treatment Center, we offer personalized treatments for face veins, including:
- Sclerotherapy
- Laser therapy
- Combination treatments customized to your skin type
Contact us today for a tailored treatment plan.
Vein Disease in Men: Recognizing Symptoms and Seeking Treatment
Varicose veins and spider veins are often wrongly considered women's issues, yet approximately 40% of men in the United States experience vein disease. Unfortunately, men frequently delay treatment, increasing the risk of complications.
Men are less likely to seek treatment early, leading to complications like:
- Leg swelling and pain
- Slow-healing ulcers
- Blood clots (DVT)
Awareness of early symptoms can lead to timely care and prevention of complications.
Risk Factors and Symptoms of Varicose Veins in Men
Men face specific risks for vein disease, including:
- Family history of venous disorders
- Age and weight-related pressure on veins
- Jobs involving prolonged standing or sitting
- Athletic activities leading to leg fatigue
Common warning signs include:
- Swelling in legs, ankles, or feet
- Heaviness, fatigue, and aching sensations
- Leg cramps, especially at night or after standing
- Skin discoloration and dermatitis around ankles
- Numbness or tingling sensations in legs
Don’t ignore these early signs—seek evaluation from our specialists.
How to Reduce Vein Problems in Men
Practical lifestyle steps can significantly help prevent or ease symptoms of vein problems:
- Regular walking or exercises focused on calf muscles
- Elevating your legs regularly, especially after prolonged standing or sitting
- Maintaining a healthy weight to ease vein pressure
- Wearing prescription-strength compression stockings
Although lifestyle changes relieve symptoms, they don’t treat the underlying issue—professional evaluation is crucial.
What Treatment Options Do Men Have?
Today, advanced and minimally invasive treatments offer men effective relief from varicose veins and venous insufficiency, including:
- Endovenous laser treatment (EVLT)
- Radiofrequency ablation
- Sclerotherapy
- Micro-phlebectomy
Men no longer have to tolerate vein-related discomfort. Early treatment ensures better outcomes and quicker recovery, with minimal downtime.
Superficial Thrombophlebitis: Symptoms, Causes, and Treatment
What is Superficial Thrombophlebitis?
Superficial thrombophlebitis (ST), often called thrombophlebitis, is a common complication of chronic venous insufficiency. This condition involves inflammation and a blood clot forming in veins close to the skin’s surface, typically causing discomfort.
Although uncomfortable, superficial thrombophlebitis is usually not dangerous. However, it's commonly mistaken for the more serious deep vein thrombosis (DVT), which requires immediate medical attention.
Superficial Thrombophlebitis (ST) vs. Deep Venous Thrombosis (DVT)
Understanding the difference between superficial thrombophlebitis and DVT is crucial:
- Superficial Thrombophlebitis (ST):
- Occurs in veins near the skin surface.
- Causes swelling, redness, warmth, and tenderness.
- Usually not life-threatening and rarely leads to severe complications.
- Deep Venous Thrombosis (DVT):
- Affects deeper veins, typically in the legs.
- Primarily causes swelling and pain but lacks redness and surface inflammation.
- Can lead to pulmonary embolism (PE), a dangerous condition where a blood clot travels to the lungs.
If experiencing symptoms, it’s important to consult a specialist for accurate diagnosis and treatment.
Symptoms of Superficial Thrombophlebitis
Common vein symptoms indicating superficial thrombophlebitis include:
- Redness along affected veins
- Tenderness or pain upon touch
- Warm skin over swollen veins
- Visible swelling and discomfort
These symptoms typically improve with proper treatment.
Effective Treatments for Superficial Thrombophlebitis
Treatment options to relieve discomfort and inflammation include:
- Warm compresses to reduce swelling and soothe pain
- Anti-inflammatory medications
- Elevation of the affected limb
- Wearing compression stockings to support vein health
In persistent or severe cases, consult our vein specialists at New York Vein Treatment Center for advanced treatment options.
Symptoms of DVT in the Legs: Know the Warning Signs
Deep Vein Thrombosis (DVT) is a condition where a blood clot forms in a deep vein, typically in your legs. Understanding the symptoms of DVT in the legs is vital for early treatment and preventing serious complications.
Common Symptoms of DVT in the Legs
Deep vein thrombosis doesn't always cause noticeable symptoms. However, you should watch for these common signs:
- Leg swelling (usually one leg affected)
- Pain or tenderness, especially when standing or walking
- Warmth or redness on the skin
- Feeling of heaviness or fatigue in your leg
- Skin discoloration (bluish or reddish tones)
DVT Complications You Need to Know
Recognizing symptoms of DVT early can help prevent serious issues like:
- Pulmonary embolism (PE): Occurs when part of a clot breaks free and travels to the lungs, causing a blockage—a medical emergency.
- Post-thrombotic syndrome (PTS): A long-term complication causing chronic pain, swelling, skin discoloration, and ulcers. About 60% of DVT patients may develop PTS.
Each year, nearly 900,000 Americans experience venous thromboembolism (VTE)—which includes DVT and PE. Prompt diagnosis and treatment significantly reduce these risks.
DVT Risk Factors: Who’s at Higher Risk?
Several factors increase your chances of developing DVT:
- Family history of blood clots
- Blood clotting disorders (hypercoagulability)
- Long periods of immobility (plane flights, hospitalization)
- Recent surgery, trauma, or injury
- Advanced age (over 60 years)
- Obesity or being overweight
- Smoking
- Pregnancy or recent childbirth
- Cancer and chemotherapy
- Hormone therapy or birth control pills
What Causes DVT in the Legs?
DVT usually occurs due to three main reasons:
- Slow or abnormal blood flow: Long immobility (hospital stays, travel).
- Vein injury: Trauma or surgery damaging vein walls.
- Hypercoagulability: Blood conditions causing excessive clotting.
Effective Treatments for DVT in Legs
Prompt medical treatment of DVT is crucial. Typical treatment options include:
- Blood-thinning medications (anticoagulants) to prevent clot enlargement and reduce new clots.
- Thrombolysis and thrombectomy: Minimally invasive procedures to dissolve or remove clots.
- Inferior vena cava (IVC) filters: Used when blood-thinning medications aren't suitable; catches blood clots before they reach the lungs.
When Should I See a Doctor for Symptoms of DVT?
Seek immediate medical care if you experience persistent or worsening symptoms of DVT in the legs:
- Severe leg swelling and pain
- Sudden or progressive redness and warmth
- Symptoms interfering with your daily routine
Delaying treatment can lead to severe complications, permanent vein damage, and nerve injury.
Charley Horse Treatment: Effective Relief for Painful Leg Cramps
Experiencing frequent Charley horses or leg cramps can significantly impact your quality of life. While occasional cramps may seem harmless, persistent Charley horses—especially at night—often signal underlying conditions such as venous insufficiency, which require medical attention.
Charley Horse or Leg Cramps: What's Causing Your Pain?
A Charley horse is a sudden, painful muscle spasm, typically occurring in the calf or thigh. Persistent Charley horses at rest or during sleep are frequently linked to superficial venous insufficiency, a condition affecting blood circulation in your legs.
When circulation is impaired, your muscles accumulate waste products (end-metabolites). These metabolites irritate nerve endings, lowering the muscle contraction threshold, causing frequent, painful spasms.
Common triggers for Charley horses include:
- Lying down or resting (especially at night)
- Minimal movements after periods of inactivity
- Prolonged sitting, such as driving long distances
Proper Charley horse treatment begins with identifying and addressing underlying circulation issues.
Leg Pain: Is It Related to Venous Insufficiency?
Chronic leg pain often indicates venous problems. With venous insufficiency, leg pain typically:
- Worsens with prolonged standing or sitting
- Improves temporarily with walking or elevation
- Intensifies later in the day and in hot weather
- May cause initial discomfort upon walking ("venous claudication"), easing after a few steps, then worsening again with prolonged walking
Unlike arterial claudication, which involves sudden calf cramping during activity, venous claudication tends to gradually intensify around the ankles, relieved by rest.
When Should I Go to the Doctor for Charley Horse Treatment?
Seek professional Charley horse treatment if:
- Frequent leg cramps disrupt your sleep or daily activities
- Pain becomes persistent, sharp, or burning
- Leg cramps occur frequently without apparent cause
Early diagnosis and proper treatment can prevent complications, such as sensory neuropathy or permanent nerve damage, and significantly improve your quality of life.
Effective Charley Horse Treatment Options
At New York Vein Treatment Center, our specialists offer personalized treatments targeting the underlying cause of your leg cramps:
- Venous insufficiency evaluation
- Minimally invasive procedures to restore healthy circulation
- Compression therapy to ease symptoms and reduce swelling
- Lifestyle recommendations for long-term symptom management
Don't ignore persistent leg cramps—contact our specialists today.
Why Choose New York Vein Treatment Center for Charley Horse Treatment?
Our specialists, led by Dr. Khitin—an expert in venous disorders, phlebology, and cardiovascular and thoracic medicine—provide comprehensive care throughout Manhattan, Brooklyn, and NYC.
Schedule your consultation today and experience relief from your Charley horse pain.
Swelling in Feet Specialist: Expert Care for Leg and Foot Swelling
If you're experiencing persistent swelling in your feet or calves, consulting a swelling in feet specialist can help identify underlying issues like venous insufficiency. At New York Vein Treatment Center, our specialists provide expert care throughout Manhattan, Brooklyn, Queens, Staten Island, and surrounding NYC areas.
When Should I Be Worried About Swelling in My Feet?
Persistent swelling in your feet or calves, especially accompanied by nighttime leg pain, could indicate untreated venous insufficiency. Early intervention can prevent severe complications, including:
- Sensory neuropathy (nerve damage)
- Persistent numbness or loss of sensation
- Chronic pain, including burning sensations
If swelling impacts your daily routine or quality of life, schedule a consultation with our swelling in feet specialists promptly.
Swelling in Calf: Understanding Edema
Calf swelling, medically known as edema, due to venous insufficiency, is often mistaken for swelling caused by heart or kidney issues. However, venous-related swelling differs significantly:
- Caused by improper fluid distribution, not fluid retention.
- Diuretics ("water pills") typically ineffective and not advisable.
- Accurate diagnosis by a specialist is critical to proper treatment.
Calf Cramps: Why Do They Occur?
Calf cramps at rest, commonly known as "Charley horses," are often symptoms of underlying venous insufficiency. These cramps occur due to circulation issues that cause waste products to accumulate in muscle tissue, triggering painful spasms—especially while resting or lying down.
Symptoms include:
- Painful muscle spasms at night
- Sharp, sudden pain in calves
- Frequent nighttime disruptions due to discomfort
If frequent cramps disrupt your daily life, consult our vein specialists to explore effective solutions.
How to Reduce Swelling in Feet?
Reducing swelling effectively involves treating the root cause rather than just the symptom. Specialists at New York Vein Treatment Center recommend the following strategies to manage symptoms and improve circulation:
- Regularly elevate legs above heart level
- Engage in moderate exercise, such as walking
- Wear prescription-strength compression stockings
- Maintain a healthy weight and balanced diet
Professional treatment may also include minimally invasive procedures targeting venous insufficiency for lasting relief.
Why Choose Our Swelling in Feet Specialists?
Dr. Khitin, an expert in venous disorders, phlebology, and cardiovascular and thoracic medicine, leads our experienced team. Our specialists provide personalized treatment, accurate diagnosis, and effective relief from swelling and related vein issues.
Should I See a Leg Pain Doctor?
Experiencing persistent leg pain can significantly impact your quality of life. If your discomfort isn't improving and begins to affect your daily activities, consulting a leg pain doctor is important to diagnose and treat underlying conditions like venous insufficiency.
At New York Vein Treatment Center, our experienced specialists provide effective treatment for leg pain in Manhattan, Brooklyn, Queens, Staten Island, and surrounding NYC areas.
Leg Pain: Understanding Venous Insufficiency
Leg pain caused by venous insufficiency often has unique symptoms compared to other leg conditions:
- Pain is typically unrelated to physical activity or exertion.
- Discomfort may range from dull aching to sharp, piercing sensations.
- Pain usually worsens after prolonged sitting, standing, or lying down.
- Symptoms often improve temporarily when walking, due to increased blood circulation.
This condition, known as venous claudication, often intensifies around the ankles and can gradually worsen if left untreated.
Leg and Calf Cramps ("Charley Horses")
Frequent calf cramps, especially at rest or during sleep, are commonly associated with venous insufficiency. Poor blood circulation causes a buildup of waste products in muscles, lowering their contraction threshold. Even small movements can trigger severe and painful spasms.
Common signs include:
- Nighttime leg cramps disrupting sleep
- Sharp, sudden pain in calves or thighs
- Persistent discomfort at rest or lying down
Leg Swelling (Edema): A Sign of Venous Issues
Swelling in the legs or calves—known as edema—often signals venous insufficiency. Edema caused by venous issues differs significantly from swelling related to heart or kidney disease:
- Venous edema results from improper blood distribution, not fluid retention.
- Diuretics (water pills) are typically ineffective for venous-related swelling.
- Proper treatment involves targeting the underlying venous condition directly.
Consulting a specialized leg pain doctor ensures accurate diagnosis and effective treatment.
When Should I Be Worried About Leg Pain?
It's important to seek medical help if your leg pain persists, intensifies, or leads to additional symptoms like numbness or burning sensations. Persistent leg pain can indicate:
- Long-standing venous insufficiency
- Sensory neuropathy (nerve damage)
- Serious tissue damage, known as trophic changes
Ignoring these symptoms can result in permanent nerve damage and decreased sensation.
How Can a Leg Pain Doctor Help?
At New York Vein Treatment Center, our leg pain doctors specialize in diagnosing and treating venous insufficiency and related disorders. Our comprehensive approach includes:
- Precise diagnostic evaluations
- Minimally invasive treatments tailored to your condition
- Effective symptom management and preventive strategies
Should I See a Leg Swelling Specialist?
If you're experiencing persistent swelling in your legs or calves that's affecting your daily life, it's important to consult a leg swelling specialist. Chronic swelling often indicates underlying conditions like venous insufficiency, which require professional diagnosis and treatment.
At New York Vein Treatment Center, our leg swelling specialists offer expert care to patients throughout Manhattan, Brooklyn, Queens, Staten Island, and the NYC area.
Leg Swelling: Understanding Venous Edema
Leg swelling (edema) related to venous insufficiency differs significantly from swelling caused by heart or kidney conditions. Key differences include:
- Venous swelling results from improper fluid distribution, not fluid retention.
- Diuretics ("water pills") are typically ineffective for venous edema and often not recommended.
- Proper diagnosis by a specialist is essential for accurate treatment.
Understanding the specific cause of your leg swelling is critical to effective, long-term relief.
Leg Pain: How Does It Relate to Leg Swelling?
Leg pain often accompanies swelling caused by venous insufficiency, characterized by:
- Pain worsening during periods of inactivity, standing, or lying down.
- Temporary improvement with movement due to increased circulation.
- Increased discomfort later in the day or during hot weather.
- Pain in the ankles, known as venous claudication, relieved by rest.
Leg pain combined with swelling suggests advanced venous insufficiency, warranting immediate attention from a specialist.
Calf Cramps: Why They Occur with Swelling
Calf cramps, especially at night or during rest, commonly signal venous insufficiency. Poor circulation causes muscles to accumulate metabolic waste products, making them prone to spasms. These cramps, or "Charley horses," typically:
- Occur frequently at night
- Are triggered by minimal movement when resting
- Cause sharp, prolonged discomfort
If calf cramps accompany leg swelling, it's important to seek evaluation from a specialist.
When Should I Be Worried About Leg Swelling?
Be concerned about leg swelling if:
- Swelling persists despite rest and elevation.
- Pain intensifies, becomes chronic, or disrupts daily activities.
- You experience numbness or burning sensations indicating possible nerve damage.
Persistent swelling and pain indicate advanced venous insufficiency, which can lead to serious complications without proper treatment.
Effective Ways to Reduce Leg Swelling
Addressing the underlying cause is crucial for long-term relief. Specialists recommend:
- Elevating legs regularly throughout the day
- Walking or engaging in calf-focused exercises
- Wearing prescription-strength compression stockings
- Maintaining a healthy weight and active lifestyle
Professional treatment by a specialist may also include minimally invasive procedures to correct venous insufficiency permanently.
Why Choose Our Leg Swelling Specialists?
Dr. Khitin, a renowned expert in venous disorders, phlebology, cardiovascular, and thoracic medicine, leads our dedicated team at New York Vein Treatment Center. Our specialists provide personalized, effective care designed to manage your leg swelling, pain, and related venous symptoms comprehensively.
Leg Cramps Specialist
Are you experiencing frequent, painful leg cramps affecting your daily life? Persistent leg cramps, especially at night, could indicate an underlying circulation condition such as venous insufficiency. Consulting our leg cramps specialist at New York Vein Treatment Center can help you find lasting relief.
Calf and Leg Cramps: What's Causing the Pain?
Calf and leg cramps, commonly called "Charley horses," often result from impaired venous circulation. Venous insufficiency leads to poor removal of waste metabolites from your muscles, causing painful spasms.
Common characteristics of leg cramps related to vein issues include:
- Painful muscle cramps occurring at rest or night
- Sharp, sudden discomfort in calves
- Sensations like pins-and-needles or numbness (paresthesia)
- Pain relieved briefly by movement but quickly recurring
These cramps differ from muscle fatigue cramps that appear after physical exercise. Venous-related cramps are typically worse when you rest or remain inactive.
Leg Pain: Could It Be Venous Insufficiency?
Venous insufficiency often causes prolonged leg pain. You may experience:
- Aching or heavy sensations worsening later in the day
- Pain intensified by prolonged standing or sitting
- Improvement with gentle walking or elevating legs
- Discomfort intensified by warm weather conditions
If you're experiencing ongoing leg pain combined with frequent cramps, it's critical to see our specialist.
Leg Swelling: Another Sign of Vein Problems
Swelling (edema) frequently accompanies chronic leg cramps. Unlike swelling from heart or kidney disease, venous-related swelling:
- Results from improper fluid distribution rather than retention.
- Does not respond effectively to diuretic (water pills) treatments.
- Requires proper diagnosis by a leg cramps specialist for correct management.
When Should I Be Worried About Leg Cramps?
Consider seeing a specialist if your leg cramps:
- Occur frequently, particularly at rest or nighttime
- Interfere with your sleep or daily routines
- Are accompanied by persistent leg swelling, pain, or skin changes
- Gradually worsen or cause sensory changes such as numbness or burning sensations
Persistent cramps indicate possible nerve damage from untreated venous insufficiency. Early diagnosis and treatment help prevent long-term damage.
Effective Leg Cramps Treatment Options
At New York Vein Treatment Center, our specialists offer personalized treatment plans addressing the root cause of your leg cramps:
- Comprehensive venous insufficiency evaluation
- Minimally invasive vein treatments to restore healthy circulation
- Compression therapy and lifestyle recommendations for symptom relief
Our approach ensures both symptom relief and correction of underlying conditions.
Restless Leg Syndrome Treatment
If you're experiencing uncomfortable sensations in your legs at night or when resting, you may be suffering from Restless Leg Syndrome (RLS). This condition is often linked to underlying circulation problems, such as superficial venous insufficiency. At New York Vein Treatment Center, our specialists provide comprehensive restless leg syndrome treatment to help you sleep comfortably again.
Symptoms of Restless Leg Syndrome (RLS)
The primary symptom of restless leg syndrome is a strong, irresistible urge to move your legs. Common characteristics include:
- Rest triggers discomfort: Symptoms typically begin after prolonged sitting or lying down, such as during travel or bedtime.
- Movement brings relief: Walking, stretching, or shifting your legs temporarily relieves discomfort.
- Symptoms worsen at night: Sensations become more severe in the evening, disrupting sleep.
- Nighttime twitching: Often accompanied by involuntary leg movements during sleep (periodic limb movement).
People often describe RLS sensations as:
- Aching or throbbing
- Pulling or tugging
- Electric or crawling sensations
- Persistent itching beneath the skin
These sensations are generally difficult to describe and fluctuate in severity, sometimes disappearing for periods before returning.
Charley Horses and Restless Leg Syndrome
Frequent Charley horses (painful calf cramps) and leg pain at night often accompany restless leg syndrome. Persistent cramps and nighttime discomfort typically indicate advanced venous insufficiency.
Common signs include:
- Painful muscle cramps, often during rest or sleep
- Increasing severity over time, affecting sleep quality
- Sensory changes, including numbness, tingling, or burning sensations
Ignoring these symptoms can lead to further nerve damage or permanent sensory issues.
When to See a Doctor for Restless Legs?
You should see a specialist if restless legs symptoms:
- Regularly disrupt your sleep
- Interfere with daily activities and quality of life
- Are accompanied by leg swelling, pain, cramps, or changes in sensation
Prompt evaluation and treatment can help prevent complications associated with untreated venous insufficiency.
Effective Restless Leg Syndrome Treatments
At New York Vein Treatment Center, treatment involves addressing the underlying venous issues causing RLS. Our approach includes:
- Detailed venous evaluation to diagnose circulation problems
- Minimally invasive procedures to improve blood flow
- Compression therapy and lifestyle adjustments to alleviate symptoms
Our goal is not merely symptom relief but also correcting the root cause of your restless leg syndrome.
Vein Symptoms: Heaviness, Tiredness, Burning, Itching, Numbness, and Skin Pigmentation
Vein problems often reveal themselves through various uncomfortable symptoms. Recognizing these signs early and seeking prompt treatment can significantly improve your quality of life.
At New York Vein Treatment Center, we offer specialized care to effectively relieve your symptoms and address the underlying venous disease. Here's a guide to common vein symptoms:
Heaviness in Legs
A common symptom of vein disorders is a sensation of heaviness in the legs. This uncomfortable heaviness is typically caused by:
- Accumulated fluids (swelling)
- Poor circulation resulting from venous insufficiency
- Reduced nutrition and oxygen supply to muscles due to impaired blood flow
Persistent heaviness is an indication to consult a vein specialist for evaluation and treatment.
Tiredness in Legs: What Causes It?
Experiencing persistent leg tiredness, weakness, or fatigue may be signs of superficial venous insufficiency. The condition can lead to:
- Increased fluid accumulation causing heavier legs
- Poor muscle nutrition due to impaired circulation
- Early muscle exhaustion even with minimal physical activity
Don’t mistake chronic leg tiredness as a normal part of aging—it could indicate underlying vein problems requiring treatment.
Burning Sensation in Legs
If your legs feel like they're burning but your skin temperature is normal, it might signal venous insufficiency. This common sensation, while not literally burning, indicates nerve irritation from impaired blood flow.
Seek prompt evaluation if you experience:
- Burning sensations, especially in lower legs or ankles
- Increasing discomfort at night or during inactivity
Consulting our vein specialists early can help prevent more severe complications.
Itching Sensations: Another Warning Sign of Vein Disease
Itching, tingling, or a crawling sensation in the legs and ankles can result from abnormal venous circulation. This symptom occurs because:
- Reversed blood flow creates nutrient deprivation and buildup of metabolic waste.
- Skin cells can't regenerate normally, causing discomfort such as itching or tingling sensations.
Treating the underlying vein disease is critical for effective relief.
Numbness of the Legs
Leg numbness is another common sign of vein disorders. Often affecting ankles, feet, or thighs, numbness can occur due to nerve damage from chronic venous insufficiency. Common characteristics include:
- Reduced sensation in affected areas
- Difficulty sensing temperature or touch
- Tingling sensations ("pins and needles")
Early treatment of venous insufficiency can reverse symptoms and prevent permanent nerve damage.
Skin Pigmentation Changes in Legs and Ankles
Venous insufficiency frequently causes skin pigmentation around ankles and calves. Typical features include:
- Brownish-black discoloration due to iron deposits from blood leaking into surrounding tissues.
- Skin becoming thickened or hardened (fibrosis).
- Gradual appearance of discoloration as venous disease progresses.
Early intervention can prevent or reverse these pigmentation changes, restoring healthier-looking skin.
When to See a Specialist About Your Symptoms
You should consult our vein specialists if you experience:
- Persistent heaviness or tiredness in legs
- Frequent leg burning, itching, or numbness
- Noticeable skin pigmentation around the ankles
- Any symptoms interfering with daily activities or sleep
Venous Leg Ulcers Treatment
Venous leg ulcers, or venous stasis ulcers, are open wounds caused by chronic venous insufficiency—a condition in which damaged veins fail to circulate blood properly. These ulcers represent up to 80% of all leg ulcers and require specialized medical care for effective healing.
At New York Vein Treatment Center, our experts offer comprehensive venous leg ulcers treatment to patients across Manhattan, Brooklyn, Queens, Staten Island, and the surrounding areas.
What Are the Symptoms of Venous Leg Ulcers?
Common signs indicating a venous leg ulcer include:
- Swelling of the ankles or lower legs
- Dry, cracked, or scaly skin around the affected area
- Skin discoloration (brown or dark pigmentation)
- Pain, itching, or burning sensation near the ulcer
- Feeling of heaviness in your legs
- Varicose veins around the ulcer area
If you notice these symptoms, consult our specialists promptly for diagnosis and treatment.
Venous Ulcer Stages: Understanding Disease Progression
Recognizing the stages of venous ulcers can help you seek treatment earlier, preventing severe complications:
- Early Stage:
- Mild skin discoloration or rash
- Dry or itchy skin on ankles and calves
- Small, irritated patches developing on legs
- Moderate Stage:
- Visible darkening and hardening of the skin (fibrosis)
- Swelling intensifies, pain becomes persistent
- Larger wounds start to form
- Advanced Stage:
- Persistent open wounds that are slow or difficult to heal
- Increased risk of infection and serious complications
Prompt consultation with a specialist can prevent progression and promote effective healing.
What Are the Signs of Venous Ulcer Infection?
Venous ulcers can easily become infected if untreated. Watch closely for these signs of infection:
- Greenish or yellow discharge (often with foul smell)
- Redness, increased warmth, or significant swelling
- Increasing pain, tenderness, or discomfort around the ulcer
If you notice any of these signs, seek immediate medical attention, as untreated infections can become serious.
How Do You Treat Venous Leg Ulcers?
Effective venous leg ulcers treatment addresses both the wound itself and underlying venous insufficiency. At New York Vein Treatment Center, we provide specialized care using advanced, minimally invasive treatments to restore circulation, heal ulcers, and prevent recurrence.
Common treatment options include:
- Endovenous Procedures:
Minimally invasive treatments (such as Endovenous Laser Therapy and Sclerotherapy) to restore healthy circulation and reduce venous hypertension. - Compression Therapy:
Prescription compression stockings to improve blood flow and reduce swelling. - Antibiotic Therapy:
Used to treat existing infections, promoting quicker healing. - Lifestyle Adjustments:
Leg elevation, regular movement, and proper skin care to enhance healing and prevent future ulcers.
How Do You Treat Venous Leg Ulcers Effectively?
At New York Vein Treatment Center, we follow a personalized approach:
- Identify and treat the underlying venous insufficiency
- Prevent infection and complications
- Accelerate healing through targeted treatments
- Provide patient education for long-term care